Microbiology and Infectious Disease
Investigating host-microbiome interactions in health and disease
Investigating host-microbiome interactions in health and disease
The human body is colonised by a diverse community of commensal microorganisms (bacteria, fungi, viruses) with beneficial roles to human health. However, many microbial species naturally inhabiting body sites such as the skin and gut also have the potential to cause disease. In this project, we aim to integrate bioinformatics, microbiology, metagenomics (genetics and genomics) and immunology to advance our understanding of the role of the human microbiome in health and disease. A key focus of our research is developing and applying new methods for strain-level resolution and exploring how the microbiome influences the emergence of antimicrobial-resistant pathogens. Ultimately, this research could inform new therapeutic strategies to combat infections and promote microbiome-based interventions for improved health outcomes over a human lifespan.
Innovating Protein Technologies for Vaccine Design
Innovating Protein Technologies for Vaccine Design
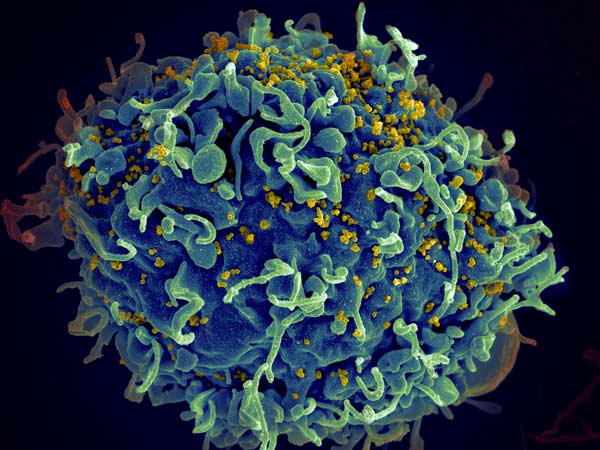
We have established an approach to accelerate vaccine development, through our Plug-and-Protect platform. A limiting factor in vaccine generation is the difficulty of turning a promising target protein into the kind of assembly that would give long-lasting disease protection. We demonstrated potent immunization towards the global health challenge of malaria. This approach is now being used by many groups against cancer and various infectious diseases, e.g. HIV, influenza, coronaviruses and other outbreak pathogens. This project will involve creating new protein antigen and nanoparticle designs to achieve the most effective and broadly protective immune responses. By inducing potent mucosal immunity, the project will contribute to developing a new generation of vaccine systems, towards protection against the most challenging diseases.
Engineering the microbiota to reduce the spread of antibiotic resistance
Engineering the microbiota to reduce the spread of antibiotic resistance
Antibiotics are crucial for the treatment of bacterial infections, but they can also cause significant collateral damage to the microbiota (de Nies et al. Nat Rev Microbiol. 2023). Antibiotics supress the growth of commensal microorganisms and at the same time select for drug-resistance. Individuals are often benignly colonized with resistant potential pathogens persisting at low levels within their microbiota, such as extra-intestinal pathogenic Escherichia coli (ExPEC). Antibiotics can lead to overgrowth of these resistant pathogens, facilitating their spread within and between individuals (Stracy et al. Science. 2022).Antibiotics can also lead to resistance genes spreading between bacteria within the microbiota through various horizontal gene transfer (HGT) mechanisms.
This overall aim of this project is to answer the important questions:
- What are the key factors that determine the level of antibiotic-induced resistance overgrowth/spread within the microbiota?
- How does antibiotic-induced pathogen overgrowth and level of HGT differ between individuals?
- Can we engineer the microbiota to prevent the spread of resistance?
To achieve this, we will use experimental approaches with synthetic and human-derived microbial communities as well as developing microscopy methods to understand the effect of antibiotics on the micro-scale biogeography of the microbiota. We will test approaches to modify the members of the microbiota to minimize antibiotic-induced pathogen overgrowth or HGT.
Characterizing structures of human monoclonal antibodies against novel P. falciparum blood-stage antigens
Characterizing structures of human monoclonal antibodies against novel P. falciparum blood-stage antigens
Monoclonal antibodies have emerged in recent years as powerful tools to guide vaccine design and potentially to directly prevent infectious disease. Plasmodium falciparum, which causes malaria, is a relatively unexplored pathogen in this area, with only a few major vaccine candidates dominating the field despite the thousands of proteins expressed by the parasite. This project aims to isolate, characterize and determine the structures of human monoclonal antibodies against known and novel P. falciparum blood-stage antigens using cutting-edge technology. This collaborative project combines the expertise of the Tan lab in isolating human monoclonal antibodies against infectious pathogens and the expertise of the Higgins lab in solving crystal structures of antibody-antigen complexes to identify new sites of vulnerability on parasites at high resolution.
Population genomics and sequencing methodologies in host-pathogen systems
Population genomics and sequencing methodologies in host-pathogen systems
Potential subprojects include: Extending methods for pangenome annotation and analysis to eukaryotic pathogens (e.g. https://www.biorxiv.org/content/10.1101/2023.01.24.524926v1).
Developing adaptive sampling and hybrid enrichment techniques for pathogen/bacteria/host sequencing (see https://www.nature.com/articles/s41587-022-01580-z.)
Linking strain/variant transmission with pathogen
genetic determinants and host epidemiology. (see: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552050/ and https://www.science.org/doi/full/10.1126/scitranslmed.abg4262)
Hepatic schistosomiasis and HIV interactions: Epidemiological approaches to pathogenesis and clinical targets
Hepatic schistosomiasis and HIV interactions: Epidemiological approaches to pathogenesis and clinical targets
Globally, HIV and schistosomiasis are leading causes of death due to infectious diseases. Despite available interventions, the infections remain uncontrolled in low-income settings causing acute and chronic morbidities. Intestinal schistosomiasis is caused by a parasitic blood fluke, most commonly of the species Schistosoma mansoni, and is predominantly found in sub-Saharan Africa. Chronic infections lead to advanced disease including liver fibrosis, portal hypertension, upper gastrointestinal tract bleeding, and severe anaemia. In the context of coinfections, severe clinical outcomes including death may be likely due to immune failure, interactions related to general fibrosis, and responses to starting antiretroviral therapy. In this project, you will have the opportunity to work with cutting-edge statistical and big data approaches alongside state-of-the art immunology to examine disease progression in the context of schistosome and HIV coinfections in arguably some of the poorest settings worldwide.
The group of Associate Prof. Chami studies schistosomiasis evaluating transmission, clinical outcomes, and treatment strategies, especially for liver fibrosis, in the SchistoTrack Cohort with the Uganda Ministry of Health. This Cohort is the largest individual-based cohort tracking individuals prospectively in the context of schistosomiasis. At Oxford, students can get exposure to computational, big data approaches to clinical epidemiology and field experience in global health research.
The group of Dr. Sereti studies HIV immune pathogenesis with a focus on inflammatory complications related to HIV and coinfections. Studies on biomarkers and how they may assist in identifying early people with HIV who may develop inflammatory and other adverse complications is currently an active area of investigation in the lab as they can also inform disease pathogenesis and new targeted interventions.
At the NIH, students can get experience in immunology research (wet lab) with optional exposure to complicated cases within a clinical setting.
Schistosomiasis pathogenesis from mice to humans
Schistosomiasis pathogenesis from mice to humans
There is a pressing need to improve the understanding of morbidity for schistosomiasis. These parasitic blood flukes afflict over 250 million people worldwide with over 700 million people at risk. For Schistosoma mansoni (a species that causes the intestinal form of schistosomiasis), untreated individuals can develop severe or functional morbidities such as enlarged livers/spleens, periportal fibrosis, oesophageal varices, anaemia, and chronic gut inflammation. The onset and progression of these morbidities is a complex interplay of host genetics and immune response, environmental factors, coinfections, and social determinants. This project is an exciting opportunity to combine work in immunology with epidemiology, providing opportunities to apply computational approaches, experimentally test mechanistic hypotheses found in humans in mice, and gain fieldwork experience in global health research. The candidate will gain skills in both wet lab work and fieldwork in Uganda. You will join multidisciplinary labs at the NIH-NIAID and Oxford.
Examining gut bacteria and bacterial pathogens to identify species combinations to prevent or treat disease
Examining gut bacteria and bacterial pathogens to identify species combinations to prevent or treat disease
The human microbiome is important for many aspects of our health and yet we currently lack the ability to modulate it for the vast majority of diseases. The key challenge is that it is a diverse ecological system, containing many strains and species of microbe, which needs new approaches and paradigms for the treatment of disease. This project will culture diverse anaerobic species of gut bacteria alongside bacterial pathogens to look for species combinations that can prevent or treat disease. The core methods will involve bacterial culture in the lab, but also germ-free mouse work to validate discoveries. A combination of ecological and evolutionary approaches will be applied to help rationally design multispecies communities that both treat disease but also avoid the evolution of resistance in pathogens. In this way, the goal is to help usher in a new set of treatments for microbiome-based diseases and reduce our reliance on antibiotics.
Characterising antibiotic-induced collateral damage in the gut microbiome
Characterising antibiotic-induced collateral damage in the gut microbiome
Antibiotics help clear an ongoing infection, but they can also cause significant collateral damage: they select for drug-resistant strains and cause dysbiosis to the commensal gut microbiota. This antibiotic-induced selection for resistance within the microbiome can facilitate the spread of resistant pathogens to extra-intestinal infections and to other patients (see our recent work: Stracy et al. Science. 2022, 375 (6583), 889-894).
This project will aim to understanding how antibiotics cause collateral damage to the microbiota leading to subsequent resistant infections. This will involve experiments with synthetic and human-derived microbial communities as well as developing microscopy methods to understand the effect of antibiotics on the micro-scale biogeography of the microbiota. The aim is to characterise the key factors that determine how antibiotics affect a patient’s resident microbial population and cause resistant opportunistic pathogens to spread. This will be used to help develop new ways to minimize the spread of antibiotic resistance both within and between patients. The project would suit applicants with a strong background in microbiology and keen interest in developing new ways to combat antibiotic resistance.
Establishing the role of low level systemic pathogens in Chronic disease
Establishing the role of low level systemic pathogens in Chronic disease
It is becoming clear that the human microbiome extends beyond the gut with bacteria and fungi found in our cells and tissues. In a range of chronic diseases, evidence is emerging that combinations of pathogens are involved in disease. Myalgic Encephalomyelitis/Chronic fatigue (ME/CFS), Chronic Lyme disease (CLD) and PANS/PANDAS have been linked to the presence of currently unknown pathogens. In CLD and PANS/PANDAS patients antibiotic treatments have been shown to improve symptoms. In ME/CFS raised levels of anti-microbial peptides, increased gut permeability and elevated levels of antibodies raised against specific bacteria have been found in blood. Data from our collaborator SoftCell biologicals indicates that high levels of wall less bacteria (L-Forms) can be cultured from blood, with high numbers of pathogens also detected by deep sequencing.
In this project we will examine blood samples of PANS/PANDAS, ME/CFS, CLD and healthy controls using metagenomic sequencing approaches. L-Form cultures will be established and subjected to anti-pathogen agents. Cell lines will be infected with L-Form organisms and thoroughly characterised using Raman microscopy and assays of mitochondrial function/dynamics. Oxford studies have shown that peripheral blood mononuclear cells from individuals with ME/CFS, multiple sclerosis and healthy controls are very different. Mitochondria also directly interact with parasites. Anti-pathogen agents and drugs which modulate mitophagy will be tested to determine if they can enhance the clearance of pathogens. The impact of Oxidative phosphorylation, glycolysis and different fuels on mitochondrial pathogen clearance will be investigated.
Investigating the evolutionary trajectories of P. aeruginosa
Investigating the evolutionary trajectories of P. aeruginosa
“Life will find a way….” In a now famous quote from the 1993 movie Jurassic Park, the “chaotician” Ian Malcolm nicely captures the essence of adaptation through evolution. But series evolutionary change often requires multiple mutations to arise – the changes arising from SNPs and indels in single genes usually amount to little more than phenotypic “tinkering”. So what would happen if we could “step on the evolutionary gas pedal” and accelerate the pace of change? Or alternatively, what would be the consequences of “slamming on the evolutionary brakes” to prevent adaptation? Well, these are just the kind of approaches that we have developed in the Welch lab, and we are applying these to look at how the opportunistic bacterial pathogen, Pseudomonas aeruginosa, adapts to the presence of infection-relevant selection pressures. Essentially, we’ve engineered the mismatch-repair system to come under the control of an inert chemical inducer, and so can “rheostatically” modulate the rate of mutation from very high (1000 x the wild-type level) to very low indeed (eliciting a state of “hypomutation” in which evolutionary change essentially grinds to a halt).
Using this system, we aim to investigate the evolutionary trajectories of P. aeruginosa when challenged with intense selection pressures e.g., in a polymicrobial environment, or upon exposure to antimicrobial agents or nutrient limitation. Project will involve elements of synthetic biology, microbiology, evolutionary biology, modelling and genomics. A stable polymicrobial culture system has recently been developed by the lab and is available for use.
Transmission of bacteria and antimicrobial resistance determinants between and among animals and humans
Transmission of bacteria and antimicrobial resistance determinants between and among animals and humans
We are interested in the transmission of bacterial pathogens and AMR determinants at multiple scales from the within-hospital level to global networks. Projects are possible on many large-scale datasets, primarily using population genomic and phylogenetic approaches to investigate these processes.
Mechanisms underlying DNA replication and cell cycle control in Plasmodium
Mechanisms underlying DNA replication and cell cycle control in Plasmodium
My group studies the human malaria parasite Plasmodium falciparum. Collaborative PhD projects can be offered in research areas centered around Plasmodium DNA biology: we are particularly interested in the molecular mechanisms underlying DNA replication and cell cycle control in Plasmodium, which replicates by an unusual method called schizogony. We are also interested in mechanisms for silencing and promoting the recombination of a family of key virulence genes called var genes - particularly the role that G-quadruplex DNA structures may play in var gene control. In fact, we have recently discovered that G-quadruplexes and their helicases have more general roles in genome stability and evolution in the malaria parasite as well.
Understanding genetic susceptibility to nontuberculous mycobacterial infections
Understanding genetic susceptibility to nontuberculous mycobacterial infections
This collaborative project between Dr. Steven Holland’s laboratory at the NIH and Dr. Lalita Ramakrishnan’s lab at the University of Cambridge will seek to understand the mechanistic basis of human susceptibility to environmental mycobacteria that are nonpathogenic to most people but can cause serious disease in individuals with specific immune deficiencies. Dr. Holland runs an international referral service that takes care of a unique cohort of patients with genetic susceptibility to nontuberculous mycobacterial infections. In the lab, they are mapping these susceptibilities and have found then to map to distinct immune genes, e.g., IRF8 and GATA-2, myeloid growth factors, IL-12R, the GTPase Rac2, to name only a few.
Dr. Ramakrishnan’s group has pioneered the optically transparent and genetically tractable zebrafish as a model for mycobacterial pathogenesis. The use of the zebrafish has enabled discoveries about TB immunopathogenesis and the genetic basis of susceptibility to TB which has led to the discovery of a variety of inexpensive, approved drugs that can be used to treat TB, often in a patient genotype-directed manner. They have also used the zebrafish to understand the mechanism of leprosy neuropathy.
Through this joint project, the two labs will work together to harness the power of the zebrafish to understand the molecular and cellular basis of the human susceptibilities identified by Holland. The student will move between humans and fish (and Bethesda and Cambridge) to uncover fundamental mechanisms of mycobacterial disease pathogenesis while acquiring mastery over the disciplines immunology, infectious diseases, genetics, molecular biology and cell biology.
Using genetic and cellular tools to identify and prioritise malaria vaccine targets
Using genetic and cellular tools to identify and prioritise malaria vaccine targets
There are more than 200 million clinical cases of malaria each year, leading to nearly half a million deaths, primarily among children in Africa. The two major tools for malaria control, antimalarial drugs and insecticides, are both seriously threatened by resistance, making the search for a highly effective malaria vaccine more urgent than ever. My lab focuses on the malaria parasite blood stages, during which parasites invade, multiply inside and consume human erythrocytes. The process of erythrocyte invasion represents a brief extracellular window in the parasite life cycle when parasites are exposed to the antibody-mediated immune system, making it a potential vaccine target. A number of vaccine-related projects are available that intersect with the interests of NIH collaborators in the NIAID Malaria Research Program, from systematic screening of new potential vaccine candidates, to deep structural understanding of current high-profile candidates, to understanding natural immunity to malaria by working with partners in endemic countries in order to inform better vaccine design. All could involve a mix of new technologies, including CRISPR/Cas9 engineering of parasite genomes, and represent an opportunity to contribute to the long-term battle against one of humanities oldest and most persistent infectious disease foes.
Characterisation of parasite cell proteomes
Characterisation of parasite cell proteomes
Apicomplexan pathogens are highly-adapted intracellular parasites of humans causing disease including malaria, toxoplasmosis and cryptosporidiosis. These parasites actively confront, subvert and defend themselves against host immune attack using a complex suite of parasite surface and secreted proteins that hijack immune signalling pathways. Moreover, transmission and generation of genetic novelty occurs in definitive hosts where differentiation into sexual parasite forms occurs. Relatively little is known, however, of the molecules and processes that drive these events, particularly during the sexual stages of parasite development. This project will use new methods in in vitro culture of sexual development in Toxoplasma, advanced methods for global spatial characterisation of parasite cell proteomes in order to identify specific proteins thought to be implicated in these interactions, and then utilise CRISPR/cas9 mutagenesis tools to engineer pools of strains deficient in these specific proteins. By assaying mutant pools both in vitro, and through the definitive host we will identify proteins and processes required for sexual stage conversion.
Structure and dynamics of bacterial chemotaxis signalling array by cryoEM
Structure and dynamics of bacterial chemotaxis signalling array by cryoEM
Bacterial chemotaxis response is crucial for colonization and infection, and the signal transduction systems that mediate such responses are potential new targets for antimicrobial drug development. Such system has emerged as a paradigm for understanding the principles of intracellular signal transduction both in bacterial and eukaryotic cells. In bacterial cells, hundreds of basic core signalling units consisting of three essential components, the chemoreceptors, the histidine kinase and the adaptor protein, assemble into a two-dimensional lattice array which allows cells to amplify and integrate many varied and possibly conflicting signals to locate optimal growing conditions. We aim to determine the structure and dynamics of the chemotaxis signalling arrays using state-of-the-art cryo-electron microscopy and tomography. We will take both in vitro and in situ structural approaches and combined with large-scale all atom molecular dynamic simulations. The ultimate goal is to assemble a time-resolved molecular movie of the entire signalling pathway in bacterial chemotaxis at an atomic level.
Host-parasite interactions in parasitic diseases, such as malaria
Host-parasite interactions in parasitic diseases, such as malaria
The Higgins laboratory are expert in the structural studies of host-parasite interactions in parasitic diseases such as malaria. They study how interactions at the heart of processes such as erythrocyte invasion are mediated. They explore how parasite surface proteins manipulate the human immune system. They examine antibodies produced in response to human vaccination and determine how these function, and they use this information to design improved vaccine components.
To discuss possible projects, contact: matthew.higgins@bioch.ox.ac.uk
Single cell proteomic and transcriptomic analysis of patients with monogenic forms of IBD
Single cell proteomic and transcriptomic analysis of patients with monogenic forms of IBD
Inflammatory bowel disease (IBD) encompasses two major diseases Crohn’s disease and ulcerative colitis. A subgroup of patients develop extreme phenotypes of intestinal inflammation due to rare monogenic defects. This includes several forms of immunodeficiency with diverse functional pathogenic mechanisms. Those defects inform on the importance of antimicrobial activity, hyperinflammatory responses and immune regulation. We investigate children with very early onset of intestinal inflammation using whole genome or whole exome sequencing to discover novel high impact genes and analyse the involved signaling pathways in vitro, in situ and in vivo. We like to understand the pathogenesis of rare “orphan” diseases to develop better treatment options for those disorders and improve understanding of pathogenic mechanisms of IBD as a whole.
The project will focus on single cell proteomic and transcriptomic analysis of patients with monogenic forms of IBD in order to understand functional mechanisms of monogenic IBD, to understand cellular communication and to identify novel therapeutic targets to induce cellular antimicrobial activity in order to maintain and reinstall intestinal mucosal barrier function.
Smartphone based image analysis for malaria diagnosis
Smartphone based image analysis for malaria diagnosis
Malaria is a major burden on global health with about 200 million cases worldwide, and 600,000 deaths per year. Inadequate diagnostics is a major barrier to effective management of cases and elimination of the disease. The current gold standard method for malaria diagnosis is light microscopy of blood films. About 170 million blood films are examined every year for malaria, which involves manually identifying and counting parasites. However, microscopic diagnostics are not standardized and depend heavily on the experience and skill of the microscopist, many of whom work in isolation, with no rigorous system in place for maintenance of their skills. For false negative cases this leads to incorrect diagnosis with unnecessary use of antibiotics, a second consultation, lost days of work, and in some cases progression into severe malaria. For false positive cases, this results in unnecessary use of antimalarial drugs and side effects.
To improve malaria diagnostics, the Lister Hill National Center for Biomedical Communications, an R&D division of the U.S. National Library of Medicine, NIH and Mahidol-Oxford Tropical Medicine Research Unit, University of Oxford, in Bangkok, Thailand are developing a fully automated low-cost system that uses a mobile phone and standard light microscope for parasite detection and counting on blood films. Compared to manual counting, automatic parasite counting is more reliable and standardized, reduces the workload of the malaria field workers and reduces diagnostic costs. To count parasites automatically, the system uses image processing methods to find cells infected with parasites in digitized images of blood films. The system is trained on manually annotated images and machine learning methods then discriminate between infected and uninfected cells, detect the type of parasites that are present, and perform the counting. The system uses a regular smartphone and digital images acquired on standard light microscopy equipment making it ideal for resource-poor settings.
This PhD project will develop and test this system for real-world use for malaria diagnosis. It will include optimisation of the system at NIH and testing of the system in the field at MORU including the smartphone application interface and performance, the system for connecting the smartphone to standard light microscopes, development of a core set of performance metrics for the application, field testing of the entire system for malaria diagnosis together with government healthcare workers and National Malaria Control Programme staff, structured interviews to gather feedback on the system and its potential role in malaria diagnosis in different settings, a formal field trial of the system performance and development of a system implementation guidance document for National Malaria Control Programmes.
The student will join a dynamic team of image analysis specialists at NLM and epidemiologists, modellers and clinicians at the MORU offices in Bangkok. They will spend time at field sites in malaria-endemic areas and will interact with government staff. Training will be provided at NIH on basic image analysis and smartphone application development and at MORU on malaria miscroscopy, clinical study methodology, data analysis and research ethics.
Understanding the contribution of parasite genotype to Leishmaniasis outcomes
Understanding the contribution of parasite genotype to Leishmaniasis outcomes
Leishmaniasis is an important disease caused by protozoan parasites that are transmitted by infected sand fly bites in tropical and subtropical regions. Depending on the strain of Leishmania, disease forms in humans range from localized, self-limiting cutaneous lesions to visceralizing infections that are fatal in the absence of treatment. The specific contribution of parasite genotype to disease outcome remains largely unknown. Taking advantage of a recently revealed sexual cycle that occurs during Leishmania development in the insect vector, our goal is to generate a series of hybrids between cutaneous and visceral strains that will be phenotyped in mouse models of cutaneous and visceral leishmaniasis. Each hybrid will be subjected to whole genome DNA and RNA-sequencing to follow parental allele, structural variation, including chromosome somy, gene expression, and epigenetic differences that associate with disease outcome. Experimental approaches will involve genetic manipulation of the parasite, DNA and RNAseq analysis, single cell genomics, and the application of various computational/bioinformatics methods developed to facilitate QTL and GWAS studies that identify linkage between genes and phenotypes.
Host response in Lyme disease: investigating factors associated with local control, dissemination and persistence.
Host response in Lyme disease: investigating factors associated with local control, dissemination and persistence.
Cellular and Molecular Biology of Malaria Parasites
Cellular and Molecular Biology of Malaria Parasites
Malaria remains an important global health problem; with increasing drug resistance and the lack of an effective vaccine, new therapies are needed and should be based on a rigorous understanding of parasite biology. Our NIAID lab has used a multidisciplinary approach to discover and characterize the three known ion channels in bloodstream malaria parasites. Through academic and pharmaceutical collaborations, we have also found potent inhibitors that are being pursued as new antimalarial drugs. Research projects will be tailored to the interests of the trainee and expertise available in possible collaborator labs. These projects may utilize molecular biology including CRISPR and heterologous expression, structural biology including cryoEM, biochemical methods including electrophysiology, epigenetics, and high-throughput screening for drug discovery. These and other methods are actively used in the lab. Dr. Desai has collaborators at Oxford, Cambridge, and Wellcome Sanger, depending on project.
Characterizing structures of human monoclonal antibodies against novel P. falciparum blood-stage antigens
Characterizing structures of human monoclonal antibodies against novel P. falciparum blood-stage antigens
Monoclonal antibodies have emerged in recent years as powerful tools to guide vaccine design and potentially to directly prevent infectious disease. Plasmodium falciparum, which causes malaria, is a relatively unexplored pathogen in this area, with only a few major vaccine candidates dominating the field despite the thousands of proteins expressed by the parasite. This project aims to isolate, characterize and determine the structures of human monoclonal antibodies against known and novel P. falciparum blood-stage antigens using cutting-edge technology. This collaborative project combines the expertise of the Tan lab in isolating human monoclonal antibodies against infectious pathogens and the expertise of the Higgins lab in solving crystal structures of antibody-antigen complexes to identify new sites of vulnerability on parasites at high resolution.
*This project is available for the 2021 Oxford-NIH Pilot Programme*
Forward and reverse genetic screening of macrophages and epithelial cells to identify host factors controlling nontuberculous mycobacterial infection.
Forward and reverse genetic screening of macrophages and epithelial cells to identify host factors controlling nontuberculous mycobacterial infection.
Dr. Ken Olivier (NHLBI) &
Dr. Steve Holland (NIAID)