Immunology
Discovering the hidden rules of tissue-specific responses to inflammation
Discovering the hidden rules of tissue-specific responses to inflammation
This collaboration between the Altan-Bonnet (NCI), Buckley and Coles (Oxford) labs addresses how organs generate distinct inflammatory responses despite sharing common components like immune cells, fibroblasts, and the extracellular matrix. In collaboration with additional teams from the Netherlands, and Canada, we aim to uncover the molecular, cellular, and tissue-level rules governing organ-specific inflammation.
We hypothesize that (1) organ context and cellular experience shape the perception of inflammatory signals, and (2) organ-specific hierarchies integrate responses into coordinated outcomes. Using a data-driven approach, we will combine ex vivo and in silico models of mouse and human tissues to explore these mechanisms. High-throughput robotics will generate diverse tissue models with varying sensitivities to infection or immunopathology. Multimodal datasets from these models will be analyzed using machine learning to build computational models, to guide iterative cycles of discovery.
This project will revolutionize tissue biology by creating a unified framework for understanding tissue-specific inflammation, paving the way for new treatments. We are seeking researchers with expertise in bioengineering, computer science, or immunology to join this interdisciplinary effort.
Project keywords: immunology, systems biology, biomedical engineering.
Understanding the immunoepigenetics of asthma
Understanding the immunoepigenetics of asthma
Asthma is the world’s most common chronic lung disease. It is increasing rapidly in incidence, but it is not known why. It arises from the complex interplay of genetic predispositions and the influence of environmental factors early in life, particularly early life infections with bacteria like haemophilus influenzae and with viruses like respiratory syncytial virus (RSV), and this points strongly to epigenetic changes being induced in the airway epithelium.
It has been previously hard to decipher these mechanisms, but that is now becoming possible due to the ability to obtain direct airway samples at bronchoscopy and via nasal brushings and importantly the advent of technologies allowing analysis of epigenetics on small tissue samples and even at a single cell level.
We have generated large epigenetic and immunological datasets of airway epithelium and bronchial biopsies at single cell resolution. We also have DNA methylation data from a large paediatric cohort with early life RSV. We have developed a murine model of long-term infection with haemophilus influenzae and so, for the first time, can model the interactions and consequences of early life bacterial / viral coinfection.
We aim to exploit these datasets and models to understand in detail the specific immunoepigenetic changes in asthma and early life infection in mice and humans with a view to developing targeted epigenetic therapies.
Defining the development and function of Tmic cells
Defining the development and function of Tmic cells
Our lab is interested in unconventional and innate-like cells (such as MAIT cells) and what their role is in immune protection and pathology.Tmic cells are one such cell - a recently described subset of T helper cells which are Microbially reactive, Innnate-like and Class II restricted. These cells are abundant in the human colon and marked out by high expression of CD161 – a feature normally associated with unconventional T cells – along with other evolving markers. However, as well as behaving like innate-like cells they bear conventional TCRs and are restricted by MHC Class II. They are also found in mice where they adopt a double negative phenotype over time in response to gut commensals. We think these cells are important in gut homeostasis (also other organs potentially) and we have shown they are involved in inflammation, but there are many questions as to their origin and overall functionality to be answered.
This project would explore the development of these cells using CBIR mice which over-express a commensal-reactive TCR, first by scRNASeq and scATACseq to define the steps along the pathway from conventional tissue memory to Tmic phenotype. Secondly using spatial transcriptomic methods to define their colocalization in the steady state and after challenge. Finally we will use a new in vivo CRISPR screen method (CHIME) to define the critical steps in development of Tmics and explore their functions in vivo. We will aim to compare mouse and human Tmic populations to define this novel conserved cell population and explore its role in health and disease.
Reference: https://www.nature.com/articles/s41467-022-35126-3
How do immune cell glucocorticoid responses contribute to psychiatric and autoimmune disorders?
How do immune cell glucocorticoid responses contribute to psychiatric and autoimmune disorders?
It is clear that stress responses and immunity are closely entwined, and epidemiological research shows that their complex interplay is key to the development of both psychiatric and autoimmune disorders (Teicher 2013 PMID:23982148, Dube 2009 PMID: 19188532). For example, a major component of the stress response is cortisol release, and depression is associated with hypercortisolaemia and glucocorticoid (GC) resistance. Abnormal responses to GCs likely contribute to the chronic inflammation observed in many patients with depression, as GCs can prime inflammatory responses, and GC-resistant immune cells produce increased levels of pro-inflammatory cytokines. Cytokines can act on the brain to produce the sickness-like behaviours characteristic of depression, and other aspects of GC-induced immune dysregulation (e.g. effects on neutrophils) may also play a role. Epidemiological studies show that psychological stress interacts with genetic risk to lead to depression and psychosis (e.g. Wang 2023 PMID:36717542), but the risk variants involved and the cellular mechanisms of this effect are unknown. We hypothesize that some risk variants for psychiatric disorders act through glucocorticoid responsive regulatory elements in specific immune cell subsets to lead to symptoms. We further hypothesize that by dissecting the cell subset- and context-specific effects of glucocorticoids in health and in patients, we can develop a better biomarker of impaired neuroendocine signalling in psychiatric disorders, opening the door to biomarker development and more personalised approaches to treatment in stress-responsive autoimmune and psychiatric disorders.
You would work with Dr Luis M. Franco and Dr Mary-Ellen Lynall to investigate these hypotheses using immunogenetic and functional genomic techniques, gaining training in cutting edge bioinformatics, statistical genetics, immunology, clinical phenotyping, and (if desired) wet-lab experimental approaches. You would integrate emerging genetic association results in autoimmune and psychiatric disorders with (a) in-house glucocorticoid-response datasets (see https://www.niams.nih.gov/labs/franco-lab) (b) healthy and patient bulk and single cell datasets from our laboratories.
Dr Franco's group in the Functional Immunogenomics Section at the NIAMS focuses on the immunobiology of glucocorticoid responses (e.g. Franco 2019 PMID:30674564).
Dr Lynall's group in the Dept of Psychiatry at Cambridge focuses on immunogenetic analyses and immunophenotyping in psychiatric patients and population cohorts (e.g. Lynall 2022 PMID:36243721).
Developing novel reporter systems to find novel regulators of reactive oxygen species generation
Developing novel reporter systems to find novel regulators of reactive oxygen species generation
Generation of reactive oxygen species (ROS) by the phagocyte NADPH oxidase is a critical and highly conserved antimicrobial function of myeloid immune cells such as neutrophils and monocytes. ROS production must be tightly regulated to ensure constant readiness for immune defence, while restraining inappropriate activation. A lack of ROS from this complex results in the devastating inborn error of immunity chronic granulomatous disease (CGD), characterised by recurrent infection but also autoinflammation and autoimmunity. Common hypomorphic variation in the genes encoding components of the phagocyte NADPH oxidase also drives pre-disposition to common autoimmune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Excess ROS production can, however, result in Understanding how ROS is tightly regulated is important for the development of rational therapeutics immune-mediated diseases.
Despite the elucidation of the NADPH oxidase complex structure and function, upstream regulators of ROS production remain largely undiscovered due to a lack of robust biological model systems. The Thomas Lab characterised EROS |(Essential for Reactive Oxygen Species) as an indispensable regulator of ROS generation but we believe that there are many more. Recent developments in CRISPR-Cas9 technology now allows both the introduction of precise edits (homology-directed repair, HDR) and genome-wide forward genetic screening by introducing knockout (CRISPRko) libraries. This may identify therapeutic targets in inflammatory disease. We will use CRISPR-HDR methods to endogenously tag key components of the NADPH oxidase complex with fluorescent proteins to generate reporter lines for iterative selection by flow cytometry. By screening these at genome-wide scale with CRISPRko libraries and sorting cells based on component expression, followed by functional screens using fluorescent ROS probes, we will elucidate upstream regulators of the complex expression and function. The function of these novel regulators can then be investigated and validated using primary and immortalised cells, structural biology, and selective mutagenesis. Interrogation of publicly available genomic datasets will guide ‘hit’ selection and possible therapeutic relevance.
Defining cross-species innate sensing of zoonotic pathogens
Defining cross-species innate sensing of zoonotic pathogens
The transmission of viruses between species faces significant barriers due to differences in host immune systems. A virus adapted to an animal host might not be well-equipped to evade the human immune system. However, mutations and other viral adaptations can occasionally overcome these barriers, leading to zoonotic infections. This concept is exemplified by the ongoing avian influenza pandemic which is now spread from birds to mammals, including livestock cow herds. Understanding and strengthening antiviral immunity is therefore crucial in preventing and controlling zoonotic diseases and for improving human and livestock health by, for example, driving next-generation vaccine development. The molecular and cellular mechanisms by which human cells sense and respond to infection are well characterised and known to be essential for host defence against viruses. Despite their importance as sources of food, their economic importance, and as sources of zoonotic pathogens, for the majority of livestock species these innate immune systems are relatively poorly defined.
In this project we the student will define the functions of PRRs that sense viral nucleic acids across multiple species, including sheep, cows, chickens, and ducks and compare them to humans. The project will employ loss of function assays, using CRISPR/Cas9, signalling and targeted perturb-seq experiments to understand the functions of these receptors. The project will also include a range of virus infection models, for example influenza viruses and poxviruses, to define how PRRs from these key livestock species impacts antiviral responses in the context of zoonotic infections.
Developing novel reporter systems to elucidate upstream regulators of cellular oxidative responses
Developing novel reporter systems to elucidate upstream regulators of cellular oxidative responses
Generation of reactive oxygen species (ROS) by the phagocyte NADPH oxidase is a critical and highly conserved antimicrobial function of myeloid immune cells such as neutrophils and monocytes. ROS production must be tightly regulated to ensure constant readiness for immune defence, while restraining inappropriate activation. A lack of ROS from this complex results in the devastating inborn error of immunity chronic granulomatous disease (CGD), characterised by recurrent infection but also autoinflammation and autoimmunity. Common hypomorphic variation in the genes encoding components of the phagocyte NADPH oxidase also drives pre-disposition to common autoimmune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Excess ROS production can, however, result in oxidative stress. Understanding how ROS is tightly regulated is thus important for the development of rational therapeutics immune-mediated diseases.
Despite the elucidation of the NADPH oxidase complex structure and function, upstream regulators of ROS production remain largely undiscovered due to a lack of robust biological model systems. The Thomas Lab characterised EROS (Essential for Reactive Oxygen Species) as an indispensable regulator of ROS generation but we believe that there are many more. Recent developments in CRISPR-Cas9 technology now allows both the introduction of precise edits (homology-directed repair, HDR) and genome-wide forward genetic screening by introducing knockout (CRISPRko) libraries. This may identify therapeutic targets in inflammatory disease.
We will use CRISPR-HDR methods to endogenously tag key components of the NADPH oxidase complex with fluorescent proteins to generate reporter lines for iterative selection by flow cytometry. By screening these at genome-wide scale with CRISPRko libraries and sorting cells based on component expression, followed by functional screens using fluorescent ROS probes, we will elucidate upstream regulators of the complex expression and function. The function of these novel regulators can then be investigated and validated using primary and immortalised cells, structural biology, and selective mutagenesis. Interrogation of publicly available genomic datasets will guide ‘hit’ selection and possible therapeutic relevance.
CRISPR-mediated screens for Phosphoinositide signaling in T cells
CRISPR-mediated screens for Phosphoinositide signaling in T cells
The Phosphoinositide 3-kinases (PI3Ks) are a family of lipid kinases that control diverse signalling pathways affecting gene-transcription, cellular adhesion and trafficking, autophagy and metabolism via the generation of PIP3. While some of these readouts are controlled by the evolutionarily conserved PI3K-AKT-FOXO, PI3K-AKT-mTOR axes, there is a diverse network of PI3K effectors that are less well studied, especially in lymphocytes, but which nonetheless can have profound effects on lymphocyte biology. We have recently used CRISPR/Cas9 to perform a targeted screen of PI3K effectors by generating a library that specifically targets PIP3-binding proteins. Screening for genes that affect T cell adhesion, we identified RASA3 as a key protein linking PI3K to the activation of the integrin LFA-1 and found that RASA3 is critical for T cell migration, homeostasis and responses to immunization (Johansen et al Sci Signaling 2022; Trend Immunol 2023; Front Immunol. 2021). We have now generated extended CRISPR/Cas9 libraries that target the entire PI3K-ome (including the kinases, phosphatases and all known effector proteins). Potential projects include designing and implementing new screens for downstream readouts of PI function, including autophagy, endocytosis, regulation of humoral immunity in vivo or other readouts, and/or understanding how RASA3 and Kindlin3 regulate T cell function and the signaling pathways. Interestingly, while RASA3 and Kindlin3 are both regulated by PIP3, they have opposite effects on LFA1 activity. We will use advanced imaging technologies to determine the differential effects of PI3K signalling on these two proteins.
Integrative studies for a mechanistic understanding of antiviral innate immunity and inflammation
Integrative studies for a mechanistic understanding of antiviral innate immunity and inflammation
Innate immune responses are the first line of defense against viral infection, but their inappropriate activation can cause autoinflammatory disease. The Best and Modis groups study how the host senses viruses, mounts sufficiently sensitive yet specific responses, and how this balance can be perturbed for example by disease mutations. Our work focuses largely on the roles of two key families of viral restriction factors, the TRIMs and RIG-I-like receptors (RLRs). We integrate an exceptionally broad spectrum of approaches, from in vivo work in high and maximum contain laboratories to state-of-the-art electron microscopy. This uniquely positions us to obtain a more complete understanding of virus-host interactions under physiological conditions with mechanistic insights in atomic-level detail.
This PhD project will focus on unravelling important insights into how RNA viruses are detected and targeted by their hosts. The aims of this project will apply our full complement of approaches, including electron microscopy, biochemical and cell-based assays, and in vivo work as needed to obtain a detailed mechanistic understanding of the contributions of virus-host interactions to antiviral innate immunity and virus pathogenesis. Our long-term goal is to use contribute to the design of novel therapeutics, such as antivirals, vaccine adjuvants, or immunomodulatory therapeutics, with potential applications in the treatment of infection, autoinflammatory disorders and cancer.
Our teams at the NIAID Rocky Mountain Laboratories and University of Cambridge are strongly committed to fostering a supportive and inclusive work environment in which trainees can thrive and experience the thrill of scientific discovery.
References:
Chiramel AI, Meyerson NR, McNally KL, Broeckel RM, Montoya VR, Méndez-Solís O, Robertson SJ, Sturdevant GL, Lubick KJ, Nair V, Youseff BH, Ireland RM, Bosio CM, Kim K, Luban J, Hirsch VM, Taylor RT, Bouamr F, Sawyer SL, Best SM (2019) TRIM5α Restricts Flavivirus Replication by Targeting the Viral Protease for Proteasomal Degradation. Cell Rep 27:3269 PMC8666140
Yu Q, Herrero del Valle A, Singh R, Modis Y (2021) MDA5 autoimmune disease variant M854K prevents ATP-dependent structural discrimination of viral and cellular RNA. Nat Commun 12:6668 PMCID: PMC8602431
Stoll GA, Pandiloski N, Douse CH, Modis Y (2022) Structure and functional mapping of the KRAB-KAP1 repressor complex. EMBO J 41:e111179 PMC9753469
Shannon JG, Sturdevant GL, Rosenke R, Anzick SL, Forte E, Preuss C, Baker CN, Harder JM, Brunton C, Munger S, Bruno DP, Lack JB, Leung JM, Shamsaddini A, Gardina P, Sturdevant DE, Sun J, Martens C, Holland SM, Rosenthal NA, Best SM (2023) Genetically diverse mouse models of SARS-CoV-2 infection reproduce clinical variation in type I interferon and cytokine responses in COVID-19. Nat Commun 14:4481 PMC10368652
Investigating the impact of regulatory cell therapy on local immune response in kidney allografts
Investigating the impact of regulatory cell therapy on local immune response in kidney allografts
Regulatory T cells (Tregs) have the ability to suppress allogeneic immune responses and have therefore become interesting as a possible cellular therapy. Our group is leading a phase II randomised clinical trial utilising Tregs as a cellular therapy for kidney transplant recipients.
The proposed project aims to in depth investigate the local immune response within the transplanted allograft, specifically focusing on infiltrating regulatory T cells and their local interactions with other infiltrating immune cells, utilising renal biopsy samples from the cell therapy trial. We hypothesise, that cellular therapy with regulatory T cells will result in trafficking of the Tregs cells to the allograft and creation of a local tolerogenic microenvironment.
We are proposing to utilise our unique collection of Treg treated patients’ biopsy samples employing the cutting-edge technology of spatial transcriptomics and single cell RNA sequencing to determine the cellular and molecular composition of leukocyte infiltrates in allograft biopsies, dissect cellular interactions in situ and determine Treg homing to the allograft.
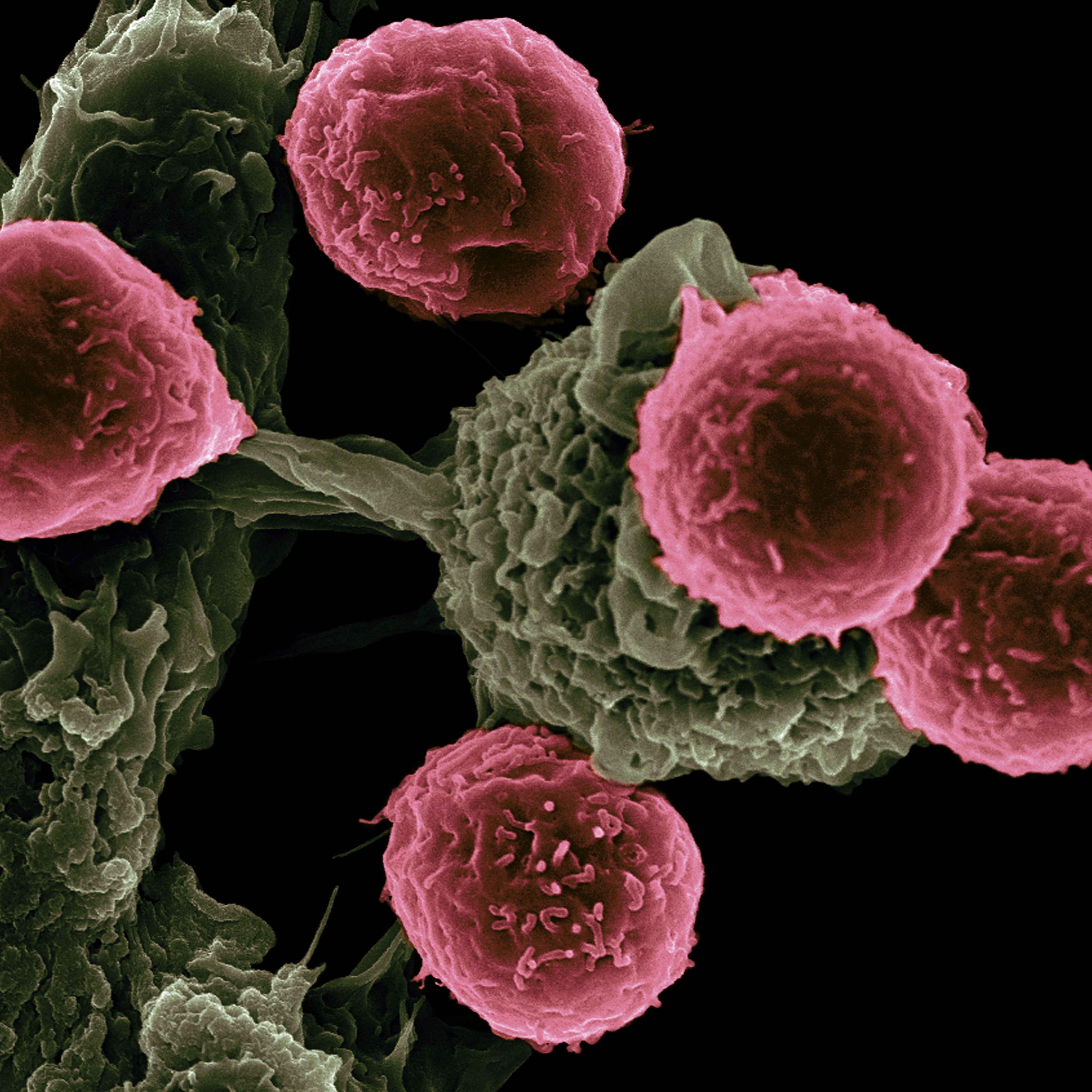
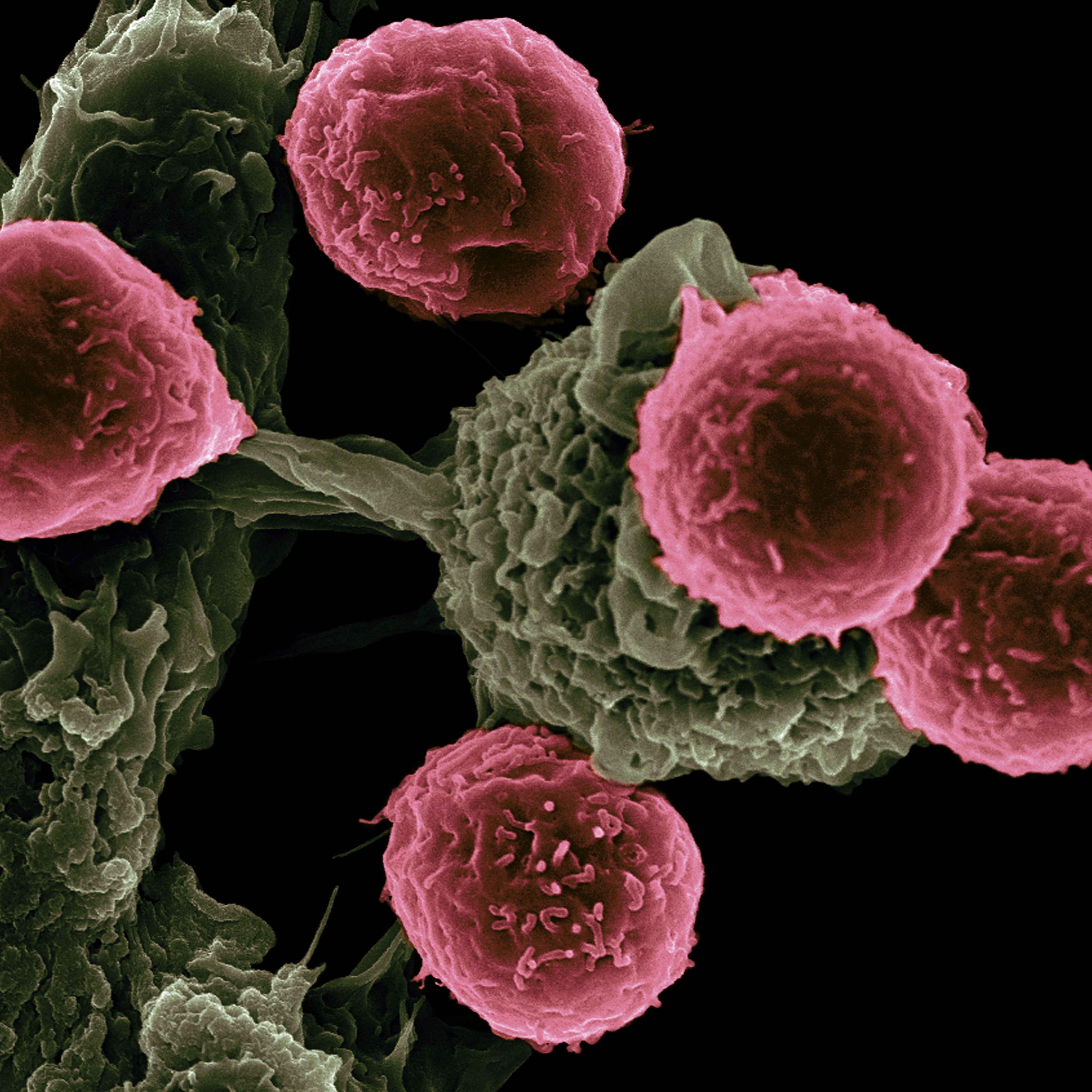
Investigating B and T cell populations in health and disease
Investigating B and T cell populations in health and disease
How are different B cell populations developmentally linked in human health and disease?
We are investigating the generation, function and plasticity of B cell populations in human health. In particular, we are interested in how different lymphocyte subsets are developmentally linked and differences in function, and therefore providing a platform to understand how B cell fate may be different in human disease. We are defining how B cells select a particular developmental pathway, and will use this information to develop methods for modulating B cell function as potential therapeutic approaches.
How can B and T cells may be therapeutically modulated across cancers and autoimmune diseases?
There is accumulating evidence for the role of both T and B cells in modulating immune responses to both solid tumours and haematological malignancies. We are investigating the contributions, function and heterogeneity of B and T cells on the immune responses to tumours and their potential role in cancer detection and treatment. We are determining the nature of B and T cell immuno-surveillance, regulation and activation across cancers and autoimmune diseases, as well as the immunological features associated with better prognosis and immunomodulation. With this, we aim to highlight novel therapeutic avenues. Our lab is affiliated with the Oxford Cancer Centre (https://www.cancer.ox.ac.uk/research/research-themes/developments-in-immuno-oncology) and non-cancer clinicians, with strong clinical links to a wide range of hard-to-treat diseases.
What is the effect of genetic and environmental variation on B and T cell fate?
Immunological health relies on a balance between the ability to mount an immune response against potential pathogens and tolerance to self. B and T cells are key to the immune response by producing antibodies and cytotoxic T cells. B/T cell clones selectively expand following antigen recognition by B and T cell receptors (BCR and TCR) respectively. BCRs are the membrane-form of antibodies and are generated through DNA recombination resulting in the potential to recognise a vast array of pathogens. Defects in the ability to mount effective B cell or T cell responses have been implicated in infectious susceptibility, impaired surveillance of cancer and immunodeficiencies, whereas a breakdown of immunological tolerance has been attributed to autoimmune diseases such as through autoantibody production and reduced numbers of regulatory B/T cells. Through integrating genomics, bulk and single-cell transcriptomics, and metabolomics data, serological, B /T cell repertoire and viromics datasets we will investigate the effect of both genetic variation and environmental factors on B cell fate, regulation, and the relationship to disease susceptibility.
Defining the role of shared T-cell receptor clonotypes in SARS-CoV-2 infection
Defining the role of shared T-cell receptor clonotypes in SARS-CoV-2 infection
T cells are a major component of adaptive immune response, continuously screening lymphoid tissues for antigen peptides presented by major histocompatibility complex (peptide/MHC or pMHC)3. These antigen peptides are recognized by T-cell receptors (TCRs). Thymocytes with a low-affinity TCRs mature into T cells and enter the lymphoid organs, where they are exposed to foreign antigen peptides by MHC molecules from antigen-presenting cells including macrophages, dendritic cells, and B-cells, during infection. When the T-cell receptors bind to antigenic peptide, T-cells are activated and undergo clonal expansion, resulting in immune response. CD8+ T cells play an important for immune response and viral clearing, but their role in protection and pathogenesis of SARS-CoV-2 remains poorly understood4. In addition to extensively studied spike protein, open reading frame 3a (ORF3a), a highly conserved protein within the Betacoronavirus subgenus, has been considered as a potential target for vaccines or therapeutics, with deletion of ORF3a resulting in decreased viral titer and morbidity. We have identified shared CD8+ T cell clonotypes responding to a ORF3a in COVID-19 infections. Importantly, shared clonotypes in severe COVID-19 infections provides a target for development of novel antiviral immunotherapies. The aim of this project is to analyse shared TCR clonotypes in ORF3a recognition and provide structural basis for the recognition of ORF3a-pMHC complex by T-cell receptors.
Elucidating the role of innate-like B lymphocytes in defense and homeostasis of host mucosal surfaces
Elucidating the role of innate-like B lymphocytes in defense and homeostasis of host mucosal surfaces
Immunity and immune-tolerance at mucosal and other barrier surfaces is vital for host survival and homeostasis with antibodies or immunoglobulins (Ig) playing a key role. However, the specific roles of B cell sub-types, particularly, the innate-like B-1 cell subset is poorly understood. The surgeon James Rutherford Morrison (1906) called the omentum in the peritoneal cavity the "abdominal policeman" and it promotes gut IgA production by peritoneal B-1 cells. IgA is the most abundantly produced antibody isotype and is known to be important for mucosal immunity. It is estimated that ~50% of IgA is derived from B-1 cells. In addition, B-1 cells are thought to be important because they make T cell-independent “natural” IgM circulating in our blood, and they can rapidly respond to mucosal perturbations such as an infection. By contrast, it will take conventional B-2 cells weeks to mount a germinal center (GC) reaction and generate antibodies that have undergone T cell-dependent affinity maturation and isotype switching. Textbooks currently do not entertain the possibility that B-1 cells can also participate in GC reactions. This project aims to challenge such an assumption. After all, B-1 cells in the gut mucosa and probably other mucosal tissues can undergo class switch recombination to IgA. However, the differentiation program that leads to this distinct pathway of IgA production is not well understood: for example, it is unknown if this process occurs outside or within GCs in mucosa-associated lymphoid tissues (MALT). Expertise on B-1 cells in the Muljo lab and the GC reaction in the Turner lab will be combined to explore this potentially paradigm-shifting research. Both wet-bench and bioinformatic research opportunities are available.
Students will learn about the fundamentals of transcriptional; epigenetic and post-transcriptional regulation; immunometabolism; in vivo CRISPR screening; CRISPR editing in primary B cells; and systems immunology. The combination of classical immunological techniques and cutting-edge, multi-disciplinary approaches will enable important discoveries to define the in vivo biology of B-1 cells. Ultimately, we seek novel insights that can be translated to inform vaccine design targeted to activate B-1 cells and/or therapeutics to inhibit their activity when necessary.
Recent publications:
Turner, D. J., Saveliev, A., Salerno, F., Matheson, L. S., Screen, M., Lawson, H., Wotherspoon, D., Kranc, K. R., and Turner, M. (2022). A functional screen of RNA binding proteins identifies genes that promote or limit the accumulation of CD138+ plasma cells. eLife, 11, e72313. PMID: 35451955; DOI: 10.7554/eLife.72313.
Osma-Garcia, I.C., Capitan-Sobrino, D., Mouysset, M., Bell, S.E., Lebeurrier, M., Turner, M. and Diaz-Muñoz, M.D. (2021). The RNA-binding protein HuR is required for maintenance of the germinal centre response. Nature Communications, 12(1):6556. PMID: 34772950; DOI: 10.1038/s41467-021-26908-2.
Wang, S., Chim, B., Su, Y., Khil, P., Wong, M., Wang, X., Foroushani, A., Smith, P. T., Liu, X., Li, R., Ganesan, S., Kanellopoulou, C., Hafner, M. and S. A. Muljo. (2109). Enhancement of LIN28B-induced hematopoietic reprogramming by IGF2BP3. Genes & Development, 33: 1048-1068. PMID: 31221665; DOI: 10.1101/gad.325100.119.
Understanding immune correlates of protective immunity
Understanding immune correlates of protective immunity
We have several lines of research that accommodate excellent PhD candidates. These revolve around the theme of RNA viral pathogens, antibodies/B-cell responses and immunodeficiencies.
The first involves understanding Immune Correlates of protective immunity, specifically which types of B-cell response and their fine specificities are important for protection against specific RNA viral pathogens (RNA viruses from HIV, HCV to Ebola) how B-cell responses to correlate with protection by vaccines to specific pathogens. The 2nd project involves using broadly neutralizing monoclonal antibodies to develop improved and novel vaccines against notoriously variable viruses. The 3rd project involves understanding how the resident virome in primary, acquired or induced immunodeficiencies leads to chronic immune activation and poor prognosis, with an emphasis on mucosal immunity.
Resolving the uncertainty in genetic diagnosis for patients with primary immunodeficiency
We have the largest world-wide collection of patients suffering from rare-inherited immunodeficiency that have been whole-genome sequenced (1500+ cases). Using established analytical expertise the candidate will use novel methods to interrogate and filter potential genetic mutations, we will identify novel candidate genetic loci in patients grouped by disease phenotype or familial relationship. Candidate genetic loci will be investigated using CRISPR-editing of patient derived material (lymphoblastoid, fibroblast and iPS cell lines). Confirmatory studies at mRNA, protein and functional level will be carried out to validate the link between variant and disease.
Investigating the impact of dendritic cell-T cell interactions on autocrine complement activation in CD4 T cells
Investigating the impact of dendritic cell-T cell interactions on autocrine complement activation in CD4 T cells
In this project, we will investigate how different stimuli including IgG-immune complexes and TLR ligands affect the ability of DCs to influence T cell autocrine complement regulation. This is of relevance to our understanding of how inflammation is propagated in autoimmunity and for vaccination boost strategies.
Examining inflammasome formation using microscopy
Examining inflammasome formation using microscopy
The inflammasome consists of a cytosolic NOD-like receptor, an adaptor molecule (ASC) and an effector molecules caspase 1. Once activated the inflammasome processes inflammatory cytokines such as interleukin 1 beta (IL1B) and IL18 as well as driving an aggressive form of cell death (pyroptosis). Inflammasomme protein complexes are central to sustaining inflammation in acute diseases (like COVID-19 associated ARDS) or chronic conditions (such as Alzheimer’s Disease, Parkinson’s, diabetes, arthritis). Patients with rare autoactivating mutations in the NLR proteins have basally active inflammasomes leading to severe autoinflammatory syndromes. How inflammasome complexes form within the cell, particularly in patients with autoactivating mutations in NLRs are poorly understood.
The aims of this project are as follows:
1. Identify the molecular mechanisms by which the gain of function mutations causes constitutive activation of the NLRs
2. Determine why gain of function mutations in different NLRs (NLRP3 and NLRC4) result in differences in inflammasome cytokine production with NLRP3 biased towards IL1B and NLRC4 towards IL18
3. Visualise how gain of function mutations alter inflammasome formation by visualising the protein complexes at super resolution and atomic resolution
This project will study how the inflammasome forms using state of the art microscopy techniques including live super resolution imaging and cyroelectron microscopy tomography. The consequences of the gain of function mutations on inflammasome formation will be studied using these techniques in cell lines where the key proteins are tagged and the gain of function mutations introduced by CRISPR/Cas9 (many of which are already available within the laboratory). This work will be extended to consider cells from patients with these diseases to map back the biology and the imaging onto the cell line models.
Are metabolites generated by the microbiota key to a young immune system?
Are metabolites generated by the microbiota key to a young immune system?
To investigate how apolipoproteins modify immune cell function in innate and adaptive airway inflammatory cells
To investigate how apolipoproteins modify immune cell function in innate and adaptive airway inflammatory cells
Asthma is the world’s commonest chronic lung disease, affecting 350 million people worldwide. The advent of novel ‘biologic’ therapies targeting specific phenotypes of asthma is currently revolutionizing the treatment of patients with type 2 inflammation. However, there are no specific treatments available for the 50% of patients with type 2 low disease. The Levine group has identified a novel pathobiologic mechanism involving dysregulation of apoplipoproteins, which may play an important role in this phenotype by regulating the recruitment and function of innate and adaptive immune cells, which may have relevance for resistance to corticosteroids. Peptide mimetics of these molecules have potential as novel therapies for asthma, especially for patients with type 2 low neutrophilic inflammation. Dr Hinks group uses in vitro, murine and ex vivo human studies on highly phenotyped asthmatics to explore the biology of the inflamed airway mucosa, particularly innate and adaptive immune cells. Through this collaboration the student would use a range of techniques and a mix of wet lab science and human experimental medicine to understand the translational potential of apolipoprotein biology in human asthma.
Investigating the role of transcription factor networks in T cell immunoregulatory fate decisions
Investigating the role of transcription factor networks in T cell immunoregulatory fate decisions
Regulatory T cells expressing the FoxP3 transcription factor (Tregs) are arguably the most important naturally-occurring anti-inflammatory cells in the body and are prime candidates for cellular therapy of autoimmunity and transplant rejection. They are potently immunosuppressive, indispensable for maintaining self-tolerance and in resolving inflammation. Tregs can be induced to develop dichotomously from naïve precursors that also have the ability to differentiate into inflammatory T cell lineages. The choice of differentiation pathway (“fate decisions”) is directed by environmental signals and interplay between many transcription factors working within networks. The expression of many genes is required for a healthy immune response and this is highlighted by the discovery of many gene mutations that are associated with very early onset auto-immune disease.
Our goal is to understand how transcriptional signals from the environment are integrated in T cells to determine inflammatory versus regulatory T cell differentiation and the quality and duration of effector function. Experimental approaches will involve genomics of patients with primary immuno-deficiencies and very early onset colitis, next generation sequencing platforms (RNA-seq, ChIP-seq, Cut&Run, ATAC-seq, scRNAseq), molecular and cell biology, CRISPR genome editing and in vivo murine models.
Understanding of the mechanisms through which CD4 T helper cells and innate lyphoid cells acquire their specific protective/tissue damaging effects.
Understanding of the mechanisms through which CD4 T helper cells and innate lyphoid cells acquire their specific protective/tissue damaging effects.
Connection between metabolism and innate immunity using mitochondrial mouse mutant models and quantitative proteomics.
Connection between metabolism and innate immunity using mitochondrial mouse mutant models and quantitative proteomics.
Genetic and molecular basis of how cellular metabolism regulates immune-function
The metabolic repertoire of immune cells – which encompasses metabolic enzymes/pathways, the available nutrient sensors and metabolic checkpoint kinases, and the epigenetic programming of metabolic genes – directly enables and modulates specific immune functions. Capitalizing on a large cohort of patients suffering from rare genetic immunodeficiency that have been whole-genome sequenced, our goal is to delineate the genetic and molecular basis of how cellular metabolism regulates immune-function in human health and disease states. Experimental approaches will involve genomics, molecular biology, cell biology, immunology, and biochemistry with an aim to elucidating mechanisms that lead to new treatment approaches to inborn diseases of immunity.
Role of lysosomes in controlling immune function
Role of lysosomes in controlling immune function
The nutrient sensing and quality control linked organelles called lysosomes are best known to immunologists due to their roles in antigen presentation (dendritic cells) and in the facilitation of pathogen elimination (macrophages). Their role in the control of immunity is further recognized that inhibition of lysosomal function can promote anti-inflammatory effects by preventing the degradation of glucocorticoid receptors and conversely that impaired lysosome function in genetic lysosome storage diseases can blunt the number and function of natural killer cells. The Platt laboratory (Dept. of Pharmacology, Univ. of Oxford) investigates immune function in lysosome storage disease and the Sack laboratory (NHLBI, NIH) explores the molecular machinery controlling lysosomal homeostasis and their roles in immunity. An integrated project between the two labs, in collaboration with an NIH OxCam Scholar would be designed to enable the pursuit of an Ph.D. studying the role of lysosomes in controlling immune function.
*This project is available for the 2021 Oxford-NIH Pilot Programme*
Dissecting the role of the complosome in immune cell tissue residency
Dissecting the role of the complosome in immune cell tissue residency
Intracellular complement (the complosome) emerges as key regulator of key cell metabolic pathways in a range of (immune) cells. In consequence, perturbations in complosome activity contribute to human disease states, including recurrent infections and autoimmunity. Recent data also indicate that high complosome expression is the defining feature of tissue-resident immune cells including T cells and macrophages. In this project, we will combine pertinent mouse models and intravital imaging to address the role of the complosome in maintaining residency and sustaining function crosstalk between immune and parenchymal cells in tissues (lung/kidney/brain?) during normal homeostasis and in disease (which one?).